Olive
Founded Year
2012Stage
Dead | DeadTotal Raised
$858.8MRevenue
$0000About Olive
Olive provides healthcare revenue cycle management solutions. The company offers services for healthcare providers, including financial clearance, revenue capture, claim management, payment management, denial prevention, and analytics and reporting. Olive serves various sectors within the healthcare industry, such as physician and specialty practices, ambulatory surgery centers, clinical laboratories, and health systems. Olive was formerly known as CrossChx. It was founded in 2012 and is based in Columbus, Ohio. Olive ceased operations in October 2023.
Loading...
Olive's Products & Differentiators
Prior Authorization Suite
Olive’s Prior Authorization Suite ensures you understand the comprehensive eligibility picture for each patient, by combining End-to-End Prior Authorization and Eligibility.
Loading...
Research containing Olive
Get data-driven expert analysis from the CB Insights Intelligence Unit.
CB Insights Intelligence Analysts have mentioned Olive in 8 CB Insights research briefs, most recently on May 29, 2024.
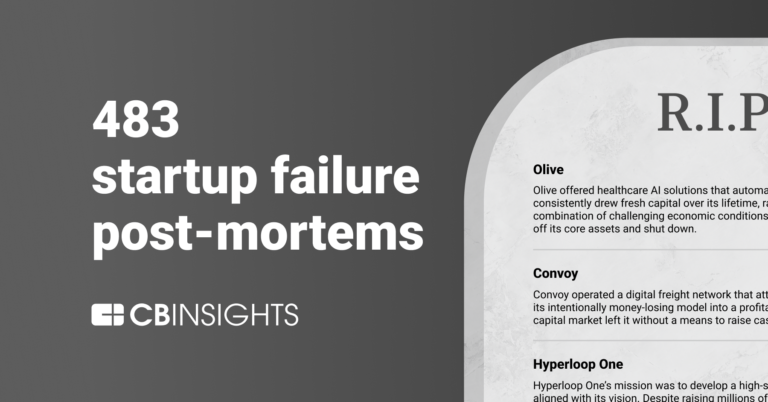
May 29, 2024
483 startup failure post-mortems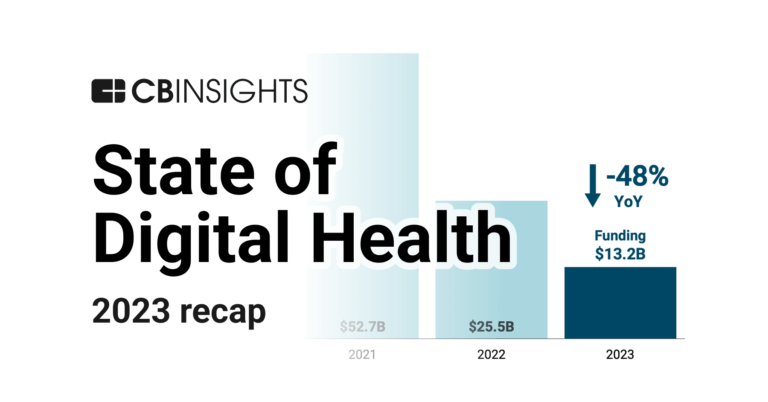
Jan 25, 2024 report
State of Digital Health 2023 Report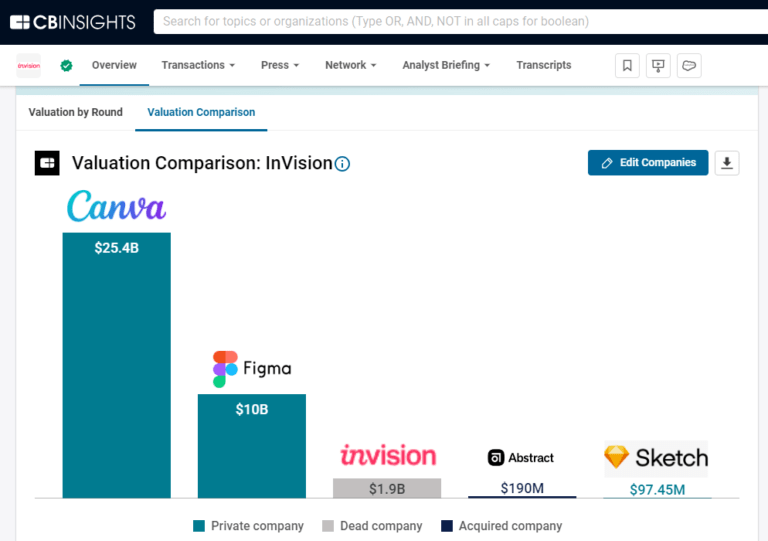
Jan 8, 2024
A $1.9B design unicorn is calling it quits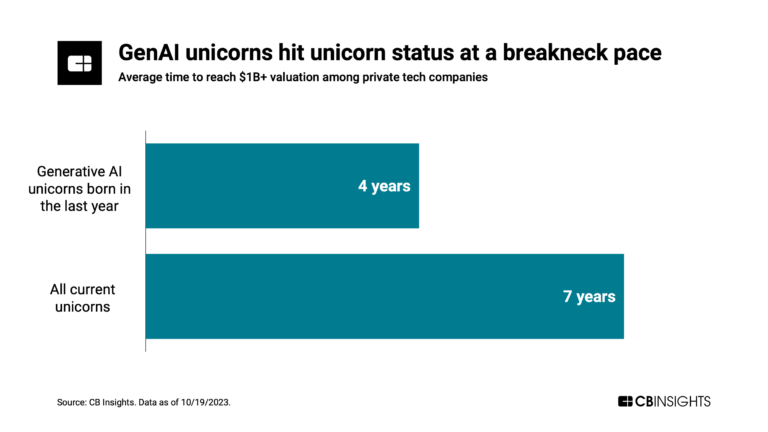
Nov 21, 2023
Has the global unicorn club reached its peak?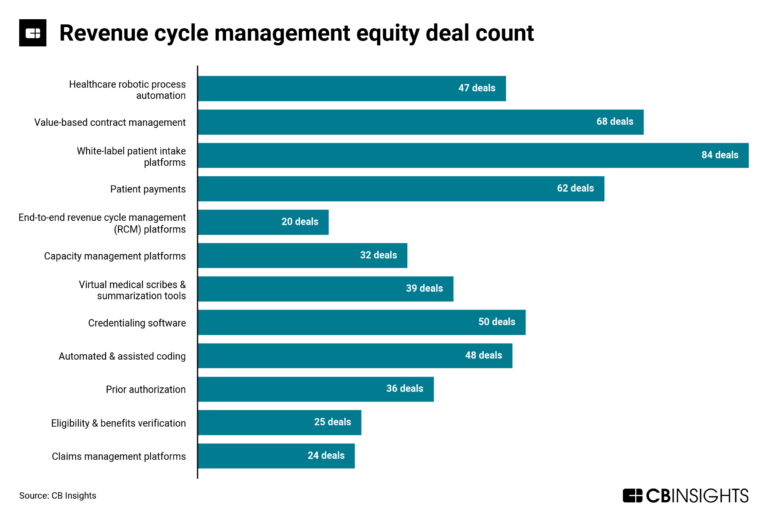
Sep 22, 2023
The revenue cycle management market map
Aug 1, 2023
The state of healthcare AI in 5 chartsExpert Collections containing Olive
Expert Collections are analyst-curated lists that highlight the companies you need to know in the most important technology spaces.
Olive is included in 7 Expert Collections, including Robotic Process Automation.
Robotic Process Automation
322 items
RPA refers to the software-enabled automation of data-intensive tasks that are low-skill but highly sensitive operationally, including data entry, transaction processing, and compliance.
Digital Health 50
450 items
The most promising digital health startups transforming the healthcare industry
Conference Exhibitors
5,302 items
Digital Health
11,419 items
The digital health collection includes vendors developing software, platforms, sensor & robotic hardware, health data infrastructure, and tech-enabled services in healthcare. The list excludes pureplay pharma/biopharma, sequencing instruments, gene editing, and assistive tech.
AI 100 (All Winners 2018-2025)
100 items
Winners of CB Insights' 5th annual AI 100, a list of the 100 most promising private AI companies in the world.
Value-Based Care & Population Health
193 items
Olive Patents
Olive has filed 53 patents.
The 3 most popular patent topics include:
- social networking services
- cubism
- modern art

Application Date | Grant Date | Title | Related Topics | Status |
|---|---|---|---|---|
6/21/2020 | 4/1/2025 | Videotelephony, Social networking services, Conservation and restoration, Teleconferencing, Machine learning | Grant |
Application Date | 6/21/2020 |
|---|---|
Grant Date | 4/1/2025 |
Title | |
Related Topics | Videotelephony, Social networking services, Conservation and restoration, Teleconferencing, Machine learning |
Status | Grant |
Latest Olive News
Sep 4, 2025
AI in Healthcare RCM: 3 Revenue Transformations AI Ushers in a New Era for Healthcare Finances: $125 Billion at Stake The healthcare industry faces a critical juncture. While delivering exceptional patient care remains paramount, financial stability is equally vital. At the heart of this delicate balance lies revenue cycle management (RCM) – the intricate process that ensures healthcare providers receive accurate and timely payment for services rendered. Despite its importance, the current RCM system is plagued by inefficiencies, costing U.S. hospitals an estimated $125 billion annually due to denied claims, billing errors, and payment delays. These losses aren’t merely financial; they directly impact staffing levels, the quality of patient services, and long-term organizational growth. But a powerful solution is emerging: artificial intelligence. AI is rapidly becoming a game-changer in healthcare RCM, offering smarter ways to handle billing, streamline workflows, and proactively identify and correct errors. By automating administrative tasks, predicting claim outcomes, and providing real-time financial insights, AI has the potential to dramatically improve RCM efficiency and unlock millions in previously lost revenue. The Three Pillars of AI-Powered RCM Transformation <h3>1. Automating the Mundane: Reclaiming Staff Time with AI</h3><p>Manual administrative tasks – from patient registration and data entry to insurance verification – are notorious time sinks and breeding grounds for errors. <strong><a href="https://www.p3care.com/rpa-medical-billing/">AI healthcare billing automation</a></strong> steps in to take over these repetitive processes, ensuring accuracy and freeing up valuable staff hours. Imagine the impact of reallocating those resources to direct patient care.</p><p>AI-powered chatbots are now handling patient billing inquiries 24/7, reducing wait times and improving patient satisfaction. According to <em>Health IT Analytics (2023)</em>, healthcare organizations leveraging <strong><a href="https://www.p3care.com/">healthcare billing AI</a></strong> have experienced a <strong>30–40% reduction in billing errors</strong>, leading to faster claim approvals and fewer denials. This isn’t just about saving money; it’s about creating a more efficient and patient-centric healthcare experience.</p><div style="background-color:#fffbe6; border-left:5px solid #ffc107; padding:15px; margin:20px 0;"><strong>Pro Tip:</strong> Don't underestimate the power of robotic process automation (RPA) within your AI strategy. RPA excels at handling structured data and repetitive tasks, making it a perfect complement to more advanced AI capabilities.</div><h3>2. Predictive Analytics: Foreseeing and Preventing Claim Denials</h3><p>Efficient claim management is the lifeblood of any healthcare provider, yet claim denials remain a persistent challenge. These denials disrupt cash flow, increase administrative costs, and create bottlenecks throughout the revenue cycle. AI-driven predictive analytics is revolutionizing how healthcare organizations manage claims, mitigating these issues and bolstering financial performance.</p><h4>How AI Predicts Claim Denials</h4><p>AI employs sophisticated algorithms and machine learning techniques to analyze historical claim data, identifying patterns that indicate a high likelihood of denial. The experts at <strong>P3care</strong> examine critical factors such as claim coding accuracy, completeness of information, and past denial trends to generate precise predictions. This allows providers to proactively correct errors *before* submission, significantly reducing the risk of rejection.</p><h4>The Benefits of Proactive Claim Management</h4><ul> <li><strong>Reduced Denials:</strong> AI helps providers avoid common pitfalls, saving time and resources.</li> <li><strong>Faster Resolution:</strong> Early identification of issues accelerates the correction and resubmission process.</li> <li><strong>Increased Approval Rates:</strong> By predicting successful claims and recommending adjustments, AI strengthens the claims submission process.</li></ul><p>Platforms like <strong>Waystar</strong> and <strong>Olive AI</strong> are leading the charge, utilizing AI-powered predictive analytics to forecast claim denials and empower providers to address issues swiftly and effectively. What impact would a 20% increase in claim approvals have on *your* organization’s bottom line?</p><h4>Proven Results: A 20% Boost in Approvals</h4><p>Hospitals that have implemented AI-driven predictive analytics have reported a remarkable <strong>20% increase in claim approvals</strong>, leading to improved cash flow and a significant reduction in administrative burdens.</p><h3>3. Revenue Optimization and Forecasting: AI as a Financial Navigator</h3><p>AI isn’t just about fixing problems; it’s about proactively optimizing revenue. By analyzing payment trends, patient behavior, and financial risks, AI empowers healthcare organizations to make smarter, data-driven decisions and improve their overall financial health.</p><h4>How AI Optimizes Revenue Streams</h4><p>AI algorithms sift through vast datasets to uncover hidden trends in patient payments, claim outcomes, and other key financial indicators. This allows healthcare providers to identify patterns, predict future cash flow, and refine their billing strategies accordingly. With AI-driven insights, hospitals and clinics can proactively adjust their approach to maximize revenue capture.</p><h4>The Advantages of AI-Powered Revenue Optimization</h4><ul> <li><strong>Improved Collection Rates:</strong> AI streamlines billing processes, making it easier to collect payments efficiently.</li> <li><strong>Enhanced Forecasting:</strong> Predictive capabilities enable organizations to plan for revenue fluctuations and avoid unwelcome surprises.</li> <li><strong>Data-Driven Decision-Making:</strong> Real-time insights empower providers to make informed decisions about pricing, payment plans, and resource allocation.</li></ul><h4>Real-World Impact: 15-25% Gains in Efficiency</h4><p>Healthcare organizations utilizing AI for revenue optimization have reported a substantial <strong>15–25% improvement in collection efficiency</strong>, alongside better overall financial management.</p> Leading AI RCM Solutions: A Landscape of Innovation Several AI-driven platforms are making a significant impact on revenue cycle management in healthcare. These tools automate processes, minimize errors, and enhance the overall efficiency of claim management and billing. Here are some prominent AI RCM services currently being adopted by healthcare providers. Key Benefits of Implementing AI RCM Tools Time Savings: Automation reduces the manual workload for administrative staff. Improved Accuracy: Minimizes errors in billing and claim submissions, reducing denials. Faster Revenue Collection: Accelerates the claims processing and approval cycle. Beyond Automation: The Broader Benefits of AI in Healthcare Billing AI’s role in healthcare billing extends far beyond simple automation; it’s fundamentally reshaping the entire process, driving improvements in efficiency, accuracy, compliance, and patient satisfaction. Here’s how P3care AI is delivering these benefits in real-time. Enhanced Efficiency: Doing More with Less One of the biggest challenges in healthcare billing is the sheer volume of administrative tasks. AI reduces this workload by automating time-consuming processes like data entry, patient registration, and insurance verification. This not only saves time but also reduces costs. According to McKinsey & Company, AI could save the healthcare sector $150 billion annually by automating administrative functions, including billing and coding. Enhanced Accuracy: Minimizing Errors, Maximizing Revenue Billing errors are a primary cause of denied claims, delaying revenue collection and adding unnecessary costs. AI-powered systems improve accuracy by analyzing historical data and identifying potential errors in real-time. Studies show AI can reduce errors by up to 40%, significantly increasing claim approval rates. By flagging coding issues or missing information before submission, AI ensures claims are accurate from the start. Ensuring Compliance: Navigating a Complex Regulatory Landscape Keeping up with evolving healthcare regulations is a constant challenge. AI helps by automatically updating billing codes and ensuring all claims comply with the latest industry standards, reducing legal risks and streamlining audits. Boosting Patient Satisfaction: A More Transparent and Positive Experience While often associated with operational improvements, AI also enhances patient satisfaction. Billing can be confusing and frustrating for patients, but AI simplifies it. AI-powered chatbots provide immediate, 24/7 responses to billing inquiries, helping patients understand their charges and payment options. This transparency fosters trust and creates a smoother experience. Addressing Integration Challenges: Connecting AI with Existing Systems Integrating AI with existing EHR/EMR systems can be complex. Legacy software may not be easily compatible with new AI tools. Successful integration requires ensuring AI solutions are compatible with existing infrastructure, potentially requiring additional time and resources. Frequently Asked Questions About AI in RCM <h3>1. What exactly is AI in revenue cycle management?</h3><p><strong>AI in revenue cycle management</strong> leverages artificial intelligence technologies – including machine learning, automation, and predictive analytics – to improve financial operations in healthcare. It streamlines billing, claims processing, and identifies revenue leaks while minimizing manual errors and administrative workload.</p><h3>2. How significantly can AI improve billing efficiency?</h3><p><strong>AI RCM improvements</strong> can reduce billing errors by 30–40% and increase claim approval rates by up to 20%. AI tools also accelerate claim processing, reduce administrative overhead, and improve overall cash flow.</p><h3>3. Is implementing AI expensive for smaller clinics?</h3><p>Not necessarily. Many <strong>AI RCM services</strong> offer scalable pricing, making them accessible even for smaller practices. While initial costs may vary, the long-term savings from reduced errors and improved collections often outweigh the investment.</p><h3>4. How does healthcare billing AI impact the patient experience?</h3><p><strong>Healthcare billing AI</strong> enhances transparency by providing 24/7 support through AI-powered chatbots and clearer billing explanations. This reduces confusion, builds trust, and improves the overall patient experience.</p><h3>5. Can AI healthcare billing automation effectively reduce claim denials?</h3><p>Yes. <strong>AI healthcare billing automation</strong> analyzes past claims, flags potential errors, and recommends corrections before submission. This proactive approach significantly lowers the chance of claim denials and improves revenue recovery.</p><h3>6. What are some of the best tools available to improve RCM efficiency using AI?</h3><p>Top <strong>AI RCM services</strong> include platforms like Olive AI, Waystar, and Kareo. These tools help <strong>improve RCM efficiency</strong> by automating routine tasks, forecasting cash flow, and ensuring compliance with billing standards.</p> AI is no longer a futuristic concept; it’s a practical, transformative tool for healthcare organizations striving to improve RCM efficiency. From automating administrative tasks to optimizing revenue and predicting claim outcomes, AI is driving smarter, faster, and more accurate financial processes. As P3Care AI healthcare billing automation continues to evolve, embracing these tools will be essential for staying competitive and financially resilient in today’s rapidly changing healthcare landscape. What steps is your organization taking to prepare for the AI revolution in healthcare finance? And how do you envision AI reshaping the patient billing experience in the years to come? Disclaimer: This article provides general information and should not be considered financial or medical advice. Consult with qualified professionals for specific guidance. Share this article with your network to spark a conversation about the future of healthcare RCM! Share this:
Olive Frequently Asked Questions (FAQ)
When was Olive founded?
Olive was founded in 2012.
Where is Olive's headquarters?
Olive's headquarters is located at 99 East Main Street, Columbus.
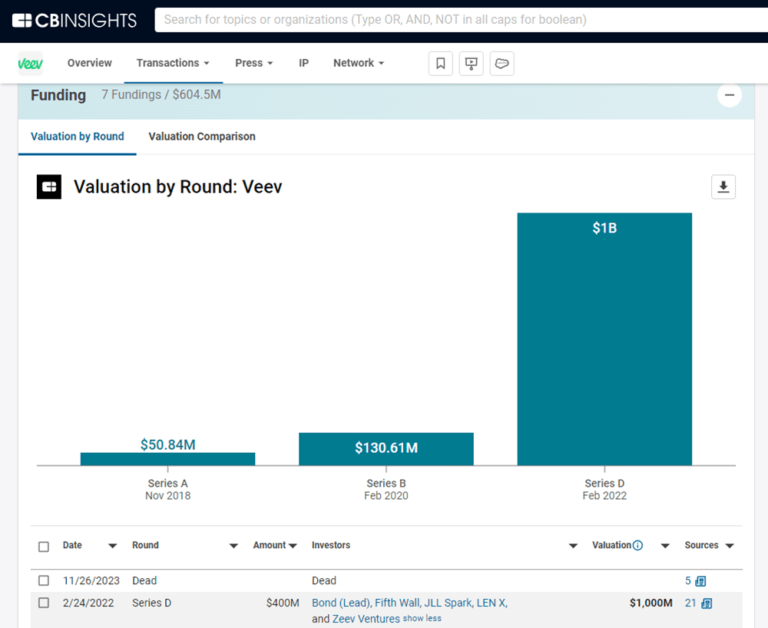
What is Olive's latest funding round?
Olive's latest funding round is Dead.
How much did Olive raise?
Olive raised a total of $858.8M.
Who are the investors of Olive?
Investors of Olive include Tiger Global Management, Vista Equity Partners, Base10 Partners, Drive Capital, General Catalyst and 16 more.
Who are Olive's competitors?
Competitors of Olive include Medical Brain, Aideo Technologies, Illumicare, FastAuth, TachyHealth and 7 more.
What products does Olive offer?
Olive's products include Prior Authorization Suite and 2 more.
Loading...
Compare Olive to Competitors

Rhyme operates as a technology company focused on automating the prior authorization process within the healthcare sector. The company provides prior authorization services, a solution to eliminate the need for prior authorizations at the point of care, and a shared dashboard for visualization and collaboration between payers and providers. Rhyme primarily serves the healthcare industry, facilitating interactions between payers and providers to improve patient care. Rhyme was formerly known as PriorAuthNow. It was founded in 2016 and is based in New Albany, Ohio.

Notable is an artificial intelligence (AI) platform that automates healthcare operations. The company offers solutions for patient engagement, workflow automation, and electronic health record (EHR) integration. Notable serves the healthcare sector with tools related to patient acquisition and retention. It was founded in 2017 and is based in San Mateo, California.

Epic is a company focused on developing healthcare software within the health informatics sector. Their main offerings include software solutions that enable medical records and facilitate patient care, as well as tools for healthcare interoperability. Epic's products primarily serve the healthcare industry. Epic was formerly known as Human Services Computing, Inc.. It was founded in 1979 and is based in Verona, Wisconsin.

Humata Health specializes in transforming prior authorizations through artificial intelligence and automation within the healthcare sector. The company offers a platform that streamlines the end-to-end prior authorization process for healthcare providers, enhancing efficiency and accuracy. Humata's solutions are designed to serve the healthcare industry, particularly in high-volume service lines such as imaging, cardiology, neurology, orthopedics, sleep studies, and surgery. It was founded in 2023 and is based in Winter Park, Florida.
AGS Health specializes in revenue cycle management (RCM) within the healthcare sector, providing services for patient access, health information management, extended business office functions, and analytics and reporting, which aim to improve healthcare revenue cycles. AGS Health serves healthcare organizations, including hospitals, health systems, and various care facilities. It was founded in 2011 and is based in Washington, DC.

AKASA provides generative AI (artificial intelligence) solutions for the healthcare revenue cycle, concentrating on financial processes within the healthcare sector. The company's offerings include automation and optimization of prior authorization, medical coding, claim status updates, and claim attachment processes, powered by generative AI trained on clinical and financial data. It serves hospitals and health systems, with a goal of improving operational efficiency and financial outcomes. AKASA was formerly known as Alpha Health. It was founded in 2018 and is based in San Francisco, California.
Loading...